At the Integrative Psychiatry Institute, we talk a lot about dietary and microbiome interventions for mental health support. Optimized nutritional requirements are complex and can be unique from person to person, depending on genetics, development, and lifestyle; it is common to hear individuals advocating for a specific botanical, multivitamin, or probiotic that worked for them. Yet there is one macronutrient, often overlooked, that stands out in promoting gut-brain health: fiber. Fiber is a crucial component of a healthy diet, offering numerous physiological and cognitive benefits. It can also be a more efficient and affordable alternative to supplements!
Understanding Fiber
Fiber is a type of carbohydrate found in plant-based foods that our bodies cannot digest alone. Instead, it passes through the digestive system relatively intact, requiring fermentation by gut microbes to break down. Soluble fiber dissolves in water to produce a gel-like substance that slows digestion; meanwhile, insoluble fiber attracts water as it moves through the digestive tract, adding bulk to stool.
While recommended intake of fiber varies depending on biological and environmental contexts, guidelines suggest aiming for around 30 grams per day for adults. However, many individuals fall short of these recommendations. Increasing fiber consumption through food choices can have a profound impact, helping to support digestive, metabolic, immune, and cardiovascular health.
The Gut-Brain Axis
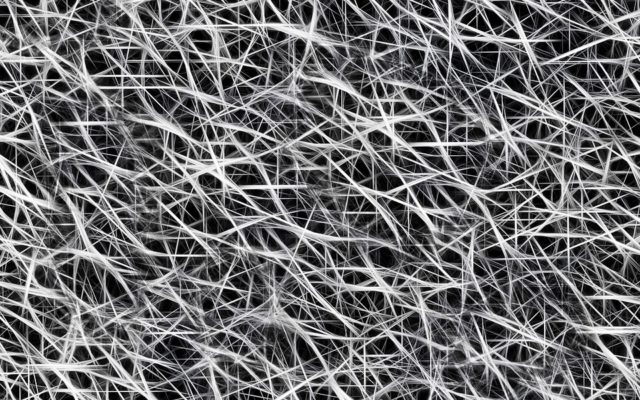
Fiber nourishes the gut microbiome and influences the gut-brain axis. You see, fiber serves as a prebiotic, acting as food for gut bacteria. This food gets broken down and absorbed into the circulation, traveling throughout the body, including to the brain where these metabolites impact neural function. Fiber may be fermented into short-chain fatty acids like acetate, butyrate, and propionate, exerting neuroprotective effects. Studies suggest that diets rich in fiber are associated with a lower risk of depression and anxiety, as well as improved stress management and cognitive function.
The intricate network between the gut and the brain, known as the gut-brain axis, highlights the relationship between gut health and mental wellbeing. Immune and nervous systems communicate bidirectionally, meaning from body to the brain and the brain to the body. The composition of the gut microbiome influences brain function and behavior through various pathways, including metabolite, hormone, and neurotransmitter production. Eating different types of plant-based foods can promote the expansion of microbial diversity; having lots of different types of gut microbes leads to a balance of metabolic byproducts and is associated with enhanced mood and cognitive function.
Putting Fiber into Practice
Nurturing a healthy microbiome through fiber-rich diets may support a holistic approach to mental health. Consider buying less processed foods. The packaging and marketing of shelf-stable items can be misleading, boasting false health benefits; it may be helpful to read nutrition labels before adding them to the cart.
Swapping out white bread for whole-grain and incorporating fresh fruits, vegetables, beans, and nuts are just a couple of ways to introduce more fiber.
Consuming high-fiber, plant-based foods will also simultaneously provide:
- Satisfying meals that regulate blood glucose levels
- Uptake of vitamins and minerals
- Exposure to additional helpful bacteria living on and in living plants (like produce)
In clinical practice, it may be enough to simply provide psychoeducation and encourage individuals to gradually increase their fiber intake, experimenting with diverse sources of fiber to amplify vitality and resilience.







